Dementia Friends USA is a global movement that is changing the way people think, act, and talk about dementia. This opportunity is open to the general public and community.
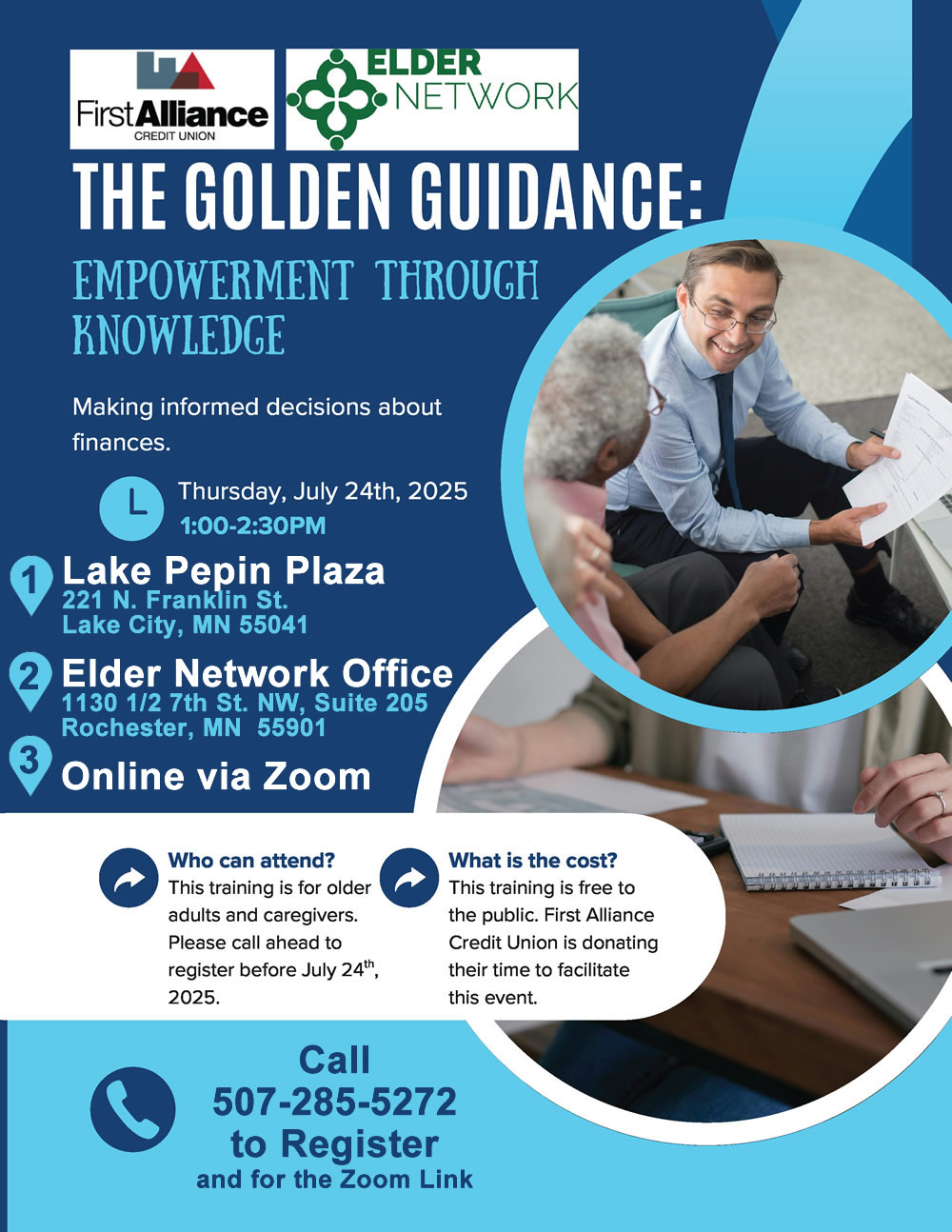
Free info session and educational follow-up on July 24, 2025
6-7pm Dementia Friends Info Sessions
7-7:30pm Interactive Education with a Cognitive Neuroscientist
Pre-registration is required (at least 24 hours in advance of the class) so that we can provide ample space and develop a certificate of completion for each participant.
There is no cost to attend, but donations will be accepted.
This opportunity will be hosted at Dodge Center Methodist Church
20 1st St. NE, Dodge Center, MN 55927
To register, contact Elder Network 507-285-5272 or beccah@elder-network.org.
Questions can also be directed to Melissa Stone – melissaS@elder-network.org.